The use of medications and surgical operations aren’t the only solution when it comes to the management or relief of pain. In the advent of chronic pain, most people quickly turn to their medicine shelf or hurry down to a drugstore, but the use of OTC medication to relieve pain often offers momentary relief only, as it doesn’t usually guarantee the discontinuity of such pain or cure what triggers it. However, we offer home remedial approaches made available by experts to help in the management of pain, and taking this supplement will guarantee relief from pain. Therapies that do not involve surgery or use of drugs are typically categorized into Physical or Sensory interventions which are specifically patient-specific and prevent non-receptive input and pain perception.
Pain can affect our quality of life and the way we think. Health and well-being coaching is an evolving practice of positive motivational counseling that leads to a change in mindset and perception about pain. These intervention techniques and approaches have been proven to be very effective in the management of pain, whether fibromyalgia or chronic pain. Various approaches that can reduce the intensity of pain and improve the quality of life of a patient include massaging, positioning, hot and cold therapy, transcutaneous electrical nerve stimulation (TENS), acupuncture, progressive muscle relaxation, and taking our Better Joint Health Supplement with CBD.
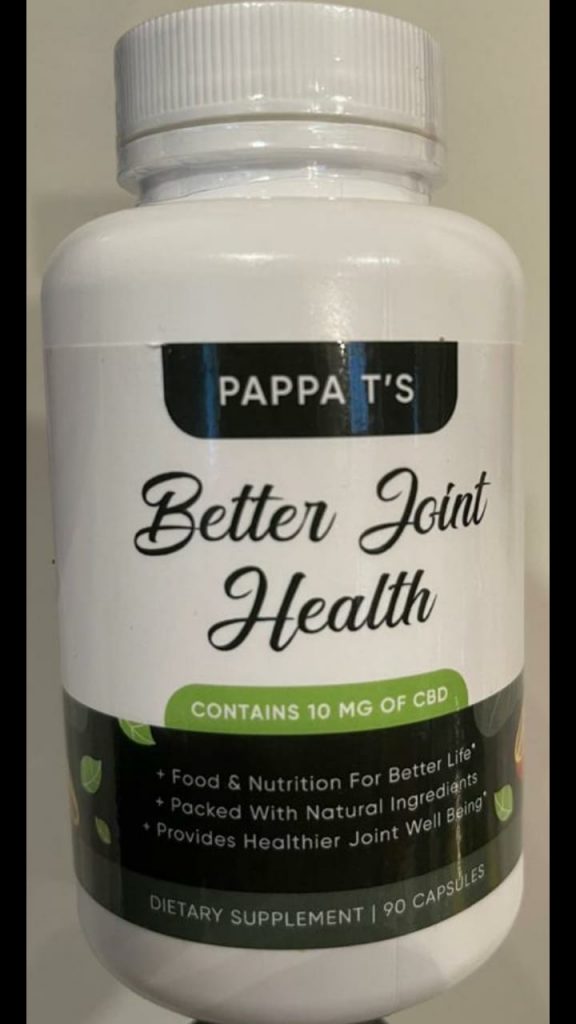
Click the image below to order a bottle
The presence of chronic pain may lead to the development of some maladaptation that will in turn disrupt the day-to-day functions, increase distress, or enhance the feeling of pain. People suffering from pain are likely to show an increased vulnerability towards a variety of illnesses such as depression anxiety disorders, or even post-traumatic stress disorder which is all triggered psychologically. Factually, the relationship between depression and pain is likely to be inseparable, and the presence of a depressive disorder has been noted as a risk factor in the transition from acute to chronic pain.
Psychological intervention approaches that are commonly adopted for the relief of pain are cognitive-behavioral therapy, mindfulness-based stress reduction, acceptance and commitment therapy (ACT), guided imagery, and bio-feedback. Chronic and acute pain have become some of the major reasons people seek medical assistance. Back pain in particular will affect almost everyone at some point in their lives. Though when medically prescribed and supervised, medication can be very helpful for the management of pain, but the misuse of opium and some over-the-counter drugs has made pain-relief alternatives desperately needed. Counseling, mindfulness coaching, exercises, Electro-therapy, and hot/cold therapy are some of the drug-free alternatives that can be very helpful in the management of pain with little or no risk recorded.
Exercise as a non-pharmacological form of pain management: Therapy involving exercises can be a very reliable way to relieve musculoskeletal pain. According to a study carried out at the University of Harvard, limiting your mobility can weaken muscles, which in turn puts more pressure on the joints and can affect posture. The study suggests that muscle weakness and poor posture can transition into a severe problem. Joint pain-relief exercises have been shortlisted to help postpone or avoid surgery by building up supportive muscles and improving flexibility.
Acupuncture as a non-pharmacological form of pain Management: One of the oldest forms of pain management techniques is the Chinese practice of acupuncture. Acupuncture makes use of tiny needles placed at specific points along the body to help lessen chronic pain. Traditional Chinese medicine explains that health is the result of a harmonious balance of the complementary extremes of “yin” and “yang” of life forces known as “qi” pronounced “chi”, and illness is said to be a resultant consequence of an imbalance of these forces. Qi is said to flow through meridians or pathways in the human body. These meridians and energy flows are accessible through three hundred and fifty acupuncture points in the body. According to traditional Chinese medical theory, acupuncture points are located on meridians, through which vital energy runs. This energy is known as “qi” or “chi.”
An acupuncturist will examine the patient and assess their condition, insert one or more thin sterile needles, and offer advice on self-care or other complementary therapies, such as Chinese herbs.
The patient will be asked to lie on their back, front, or on their side depending on where the needles are to be inserted. The acupuncturist makes use of single-use, disposable and sterile needles, as each needle is inserted, the patient may feel a very brief tingling sensation. After the needle is inserted, there is occasionally a dull ache at the base of the needle that then subsides. Acupuncture is usually relatively painless.
Sometimes the needles are heated or stimulated with electricity after insertion. The needles will stay in place for about five to thirty minutes. The number of treatments needed depends on an individual, a person with a chronic condition may need 1 to 2 treatments a week over some months even though an acute problem usually improves after eight to twelve sessions.
In a study carried out in Germany, acupuncture has been recorded to have helped in the relief of tension, body aches, and migraines. The NCCIH noted that acupuncture has been proven to help in cases of low back pain, neck pain, osteoarthritis, knee pain, headache, and migraine.
The World Health Organization (WHO) in 2003, listed several conditions in which acupuncture has been known to be effective. These included chemotherapy-induced nausea and vomiting, some gastric conditions like peptic ulcer, high and low blood pressure, painful periods, dysentery, facial pain, morning sickness, allergic rhinitis, rheumatoid arthritis, sprains, sciatica, tennis elbow, dental pain, reducing the risk of stroke, inducing labor, etc. Acupuncture can be beneficial in that it is safe when performed correctly, it has very few side effects, can be combined with other treatments, and can control some types of pain.
Massage as a non-pharmacological form of pain Management: Massaging has a lot of therapeutic benefits for chronic pain relief or management. From a deep tissue massage to a gentler technique, a massage can enhance the relaxation of muscle and sore tissues and equally lessen chronic pain. A study carried in the Annals of Internal Medicine, found that the benefits of massage in easing lower back pain may last for six months or even more.
Physical therapy as a non-pharmacological form of pain Management: Physical therapy shows how to gently move and stretch muscles and joints to strengthen them, and this helps to relieve pain. Unlike the use of a drug, physical therapy can help in treating an underlying source of pain (whether arthritis or other conditions) and alleviate chronic pain as time goes. Physical therapy may involve water therapy such as stretching muscles in a pool or whirlpool. Physical therapy also includes regular exercises and working with specialists. An article published in Annals of Internal Medicine, 2012, showed that doing home exercises taught by physical therapists was more effective for neck pain than drugs.
Hot and Cold Therapy as a non-pharmacological form of pain Management: Heat therapy promotes blood flow to areas of the body in pain due to inflammation, and allows muscles to relax. You can apply a heating pad or a heat wrap, or relax in a hot bath for the relief of pain, which can soothe the body and soul. Cold therapy can also be effective in the relief of pain. By slowing the flow of blood to a painful joint, inflammation is reduced and nerves are inhibited from quickly sending messages of pain to the brain. Applying ice, a cold wrap, or a cold pack can ease a flaring and painful joint.
Therapy for the Mind as a non-pharmacological form of pain Management: Anxiety, stress, and depression can increase chronic pain, so it’s essential not to ignore the emotional triggers of pain. Cognitive-behavioral therapy teaches how to manage thoughts, feelings and the body’s physical responses can be very effective in managing chronic pain. Bio-feedback is another method that teaches you how to control your body’s reactions to pain, while hypnosis allows deep relaxation to help with pain management.

Transcutaneous Electrical Nerve Stimulation (TENS) as a non-pharmacological form of pain Management: By electrically stimulating the area it hurts, you can help to alleviate the pain. Transcutaneous electrical nerve stimulation or TENS is the electrical stimulation technique most often used in the relief or management of pain. A small device attached to the skin sends electrical impulses to the painful area, stimulates nerves, and lessens pain as a result of it.
Bio-feedback is a non-pharmacological form of pain Management: Applied psychophysiology or better known as bio-feedback is a technique in which the patient receives extra “extrinsic” information that is not based on what the patient feels, and the information should be in real-time and biological. That is the use of real-time ultrasound biofeedback for a patient with pelvic floor muscle dysfunction or low back pain or the use of electromyography (EMG) in real-time for patients with musculoskeletal disorders. In simple words by Schawarts and Olsen, “psycho-physiology involves the scientific study of the interrelation of physiological and cognitive processes.
Guided imagery as a non-pharmacological form of pain Management: Several clinical trials have recorded a remarkable reduction in pain using guided imagery technique. Guided imagery is a technique in which an expert provokes a state of mind or mental images in a patient. As discussed by Bresler and Rossman, guided imagery involves a lot of approaches, ranging from simple visualization and direct imagery-based suggestions to metaphor and storytelling. Guided imagery has been in recent times explored exponentially in different medical settings for the management of post-operative pain, fibromyalgia, low back pain, or musculoskeletal-related pain. Those images when captured vividly may elicit a physiological response through modulations at the level of the autonomic nervous system, and such effects would result in changes of the cardiovascular, respiratory, nervous, endocrine, and even the immune system.
Conclusion
The role of non-pharmacological techniques and approaches in the management of pain is ever-changing, and even non-pharmacological and complementary therapists have an all-time high vital contribution to make for the holistic well-being of patients. Generally, these non-pharmacological approaches are relatively cost-effective with high safety profiles and low side effects. There are several pieces of evidence to support the use of patient education, cognitive behavioral therapy (CBT), relaxation, music, and other approaches to relieve pain. These therapies should be taken into consideration to help and support the standard pharmacological treatment in pain management. While medical drugs are essentially used for the treatment of the physiological and emotional (somatic) dimension of the pain, homemade remedies and non-pharmacological therapies are used for the treatment of cognitive, affective, behavioral, and socio-cultural dimensions of the pain. Non-pharmacological approaches help the patients to control their feeling, reduce the feeling of weakness, enhance their functional capacity and activity level.
Pain is an extremely complex, physical and psychological state that involves a lot of behavioral responses, thoughts, and emotions. A lot of non-physical factors such as psychological, familial and societal attitudes, life stress, cultural, spiritual and religious beliefs contribute significantly to how an individual’s experience and respond to pain. Emotional disturbances like depression and anxiety play a huge role in how we experience pain. A Myriad of studies has shown that individuals experiencing pain reported more severe pain and disability if they had anxiety, depression, or both.
Pain as defined by the International Association for the Study of Pain as “an unpleasant sensory and emotional experience associated with actual or potential tissue damage or described in terms of such damage.” Pain management pioneer, Margaret McCaffery, calls pain “whatever the experiencing person says it is, existing whenever he says it does.” Technically, both instances fail to capture pain experienced by infants and children who cannot tell what a painful damaged tissue feels like, or even where to find them.
Does it mean that infants and nonverbal children cannot or do not experience pain? Not at all. This awakening has finally led researchers to observe the behavior of infants and nonverbal children to understand their pain. There are many types of pain and each has its distinguished symptom(s).
Analyzing pain is beyond merely quantifying it. Assessment of pain should include a thorough bio-psychosocial history, review of systems, and physical examination. Whenever it is possible, physicians should ask the patient about the quality, location, character, duration, frequency, and intensity of the pain. This often helps to encourage the patient to speak in detail rather instead of asking series of questions that can easily bore them.
Interestingly, it has been found that fear of pain can cause more disability than a current situation of pain. There is a recurrent pattern of chronic pain leading to depression, and depression leading to an increase in chronic pain, thereby creating a mutually-reinforcing relationship. You don’t have to live with chronic pain or rely on a bottle of pills for the rest of your life, there are various pain management remedies to choose from. By consulting a doctor, you’re sure to find a method that works effectively to relieve pain. Music since ancient times has been used to improve well-being and reduce pain and suffering. Playing music for patients during or after surgery helps to lessen pain.
Progressive muscle relaxation is a technique whereby the participant(s) tightens and relaxes different muscles throughout the body in a progressive manner that in turn provokes a sense of relaxation and comfort. There are many indications to the use of PMR, including back pain, phantom limb pain, headache, and stress. PMR is a safe technique.
The use of biofeedback and progressive muscle relaxation techniques as initial therapy for patients without any serious pathological chronic low back and neck pain has been supported by the Global Spine Care Initiative for Communities with low and medium income. Including the Biopsychosocial (BPS) model to manage pain by targeting cognitive responses to pain and maladaptive behavior in addition to social and environmental factors may play a huge role in changing the perception of pain. BPS therapy has shown effectiveness for many physical disorders, psychiatric illnesses, and pain.
Cognitive-behavioral therapy (CBT) helps to develop an important set of coping skills intended to improve psychological functioning like behavioral activation, structured relaxation exercises, recalling and scheduling of pleasurable events, dogmatic assertive communication, and behavior pacing aimed at avoiding the prolongation and/or severity of pain. CBT for pain also addresses maladaptive thoughts about pain through a formal use of cognitive restructuring.
Mindfulness-based stress reduction: This technique enhances uncoupled awareness of both physical and psychological states because when the signal of pain cannot be established, such a detachment may change the brain response to pain. This approach aims at disconnecting the link between the sensory elements of pain and the emotional or evaluative elements of it. Using mindfulness-based stress reduction strategies such as awareness and meditation, different ideas and beliefs about pain may be perceived as an unattached event rather than a sign of an underlying matter that requires lineal and possibly maladaptive (anxious or depressive) reactions.

Acceptance and commitment therapy: This approach implies that thoughts do not have to be changed or targeted, but the responses to these thoughts may be altered in a way that the resulting negative consequences are handled. ACT approaches can improve the sense of well-being through purposeful and non-judgmental acknowledgment of mental events like emotions and thoughts facilitating acceptance of such events and enhancing the capability of the patients to maintain balance and be aware of relevant environmental and psychological factors. With this, patients may be able to modify their behaviors in a way that aligns with their goals and values instead of keep focusing on the pain. While conducting pain management, ACT can boost purposeful awareness and pain acceptance, hence diverting the focus on relieving pain.
Even though behavioral and physiological signs are helpful, they can sometimes be misleading in analyzing pain. For instance, an infant undergoing an ear examination may scream and distort facial muscle out of fear, and not pain. In a reverse manner, children experiencing continuous pain from trauma, surgery, or ailments may seem quiet and reserved, leading their medical caregivers and even parents to wrongly assume that they are sedated or relaxed. Most times, children don’t show or talk about pain because of the well-founded fear of talking to strangers, embarrassing or perturbing people around them, being given an injection, having to visit a hospital, and a host of other militating factors. Even a child going through chronic pain may seem to be playing or doing just fine as a way to distract attention from people or pain. This may be a coping mechanism for that child, but this may also lead to a misinterpretation at another time that the child is “faking pain” to avoid playing with others. Therefore, the struggle for primary care providers and parents is to be able to tell a child’s behavior and analyze whether they reflect pain or some other emotions.
Children between the age of three and seven years old are capable of describing the severity of their pain, so self-report techniques such as drawings, pictures of faces, or graded color intensities are often recommended when dealing with this age group. Pain in children between 8 years and above can be accurately analyzed using verbal or visual analog pain scales and numerical ratings. Regularly documented pain assessments are now a requirement for children in hospitals and children seeking treatment at the outpatient hospital, clinics, and emergency units. Several pain scales have been built to enhance this process, including some behavioral distress scales used for newborns, toddlers, nonverbal children, or those with communication difficulties. These scales are used to evaluate a patient’s body movements, crying, and facial expressions.
Currently, verbal numerical ratings are considered the gold standard for a reliable pain assessment. The numerical rating scale consists of numbers from zero to ten; zero represents the absence of pain and ten represents the presence of very severe pain. Still, there is an ongoing debate over the label to adopt for the rating of the highest, and the general agreement is not to use “the worst pain possible”, since children and infants can always have an imaginative picture of greater pain.
Click the image below to order your Better Joint Health Capsules to Relieve your pain and inflammations.


